| November 8, 2014 | Updated October 2024
Note from the Author:
As I revisit this post from 2014, it’s striking how much has changed since then, both in my life and in the world of mental health. PTSD remains a deeply misunderstood condition, and while there have been improvements in treatment, misdiagnosis and lack of awareness are still too common. I am sharing my story again to shed light on the struggles many face when seeking proper help for trauma, and to encourage those who are still on this difficult journey. There is hope—even when it feels like the system is failing you.
West London NHS and the Early Years of Misdiagnosis
The following is taken from my end-of-treatment assessment for trauma-focused cognitive behavioral therapy at Oxford University. These are my personal views and reflect how I felt at the time.
I was never offered PTSD treatment by any of Dr. Nick Broughton’s staff at the West London Mental NHS Trust — this included staff from Charing Cross, West Middlesex, and Chelsea & Westminster Hospitals. Despite several years of visits related to post-traumatic symptoms, I was not properly assessed.
The first time I was officially assessed for PTSD was in October 2011 by Dr. Katherine Thackeray of West Middlesex Hospital. This only happened because a senior psychologist, Dr. Richard Simpson from the Ealing Metanoia Clinic, contacted my GP at Grove Park Surgery, Dr. Hunt, and demanded I be given the PTSD assessment I was entitled to after mentioning my involvement in the 2004 Asian Tsunami and my role in the two-day search and rescue operation.
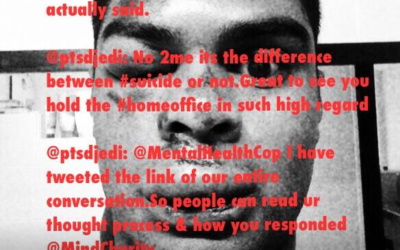
If not for Dr. Simpson’s intervention and my subsequent treatment with Dr. Jennifer Wild at Oxford University, I honestly believe I would have taken my own life. My extensive NHS West London Mental Health Trust medical records show I was never even tested for PTSD, despite multiple suicide attempts, self-harm, and a 3-4 day psychiatric ward stay at Charing Cross Hospital after which I feared for my own safety.
The Struggles of Living with Untreated PTSD
This part is extremely difficult to write. I’m not a medical practitioner—I’m a survivor of the tsunami. I was involved in carrying the dead and caring for the severely injured on Koh Phi Phi Island for 24 hours before we received outside help. What follows are my reflections from the self-assessment I completed after receiving trauma-focused cognitive behavioral therapy at Oxford University.
What kept your problems going?
There were several factors that prevented my recovery and prolonged my suffering:
- Inability to express my feelings
I struggled to articulate the severity of my experiences and the symptoms I was facing. Words felt inadequate. - Unhelpful rumination
I obsessively replayed the events, questioning why they happened, why I survived, and trying to make sense of the uncontrollable. - Personal and family turmoil
My parents’ divorce, which happened a year before the tsunami, compounded my emotional state. Returning to an uneasy home life made opening up to them impossible. The cultural gap between me and my parents only exacerbated this. - Isolation and confusion
After the tsunami, I was lost in London. I didn’t know how to cope or where to turn. Moving to Japan soon after isolated me further in some respects, though work and friendship provided temporary relief. - Ignorance of PTSD symptoms
I didn’t realize I was suffering from PTSD. I couldn’t describe the symptoms well enough for a quick 5-minute GP appointment. I was often misunderstood, dismissed, or given the wrong advice.
The Misdiagnosis and Impact on My Life
The NHS system, unfortunately, failed me time and again. I often found myself at the GP or hospital in a state of crisis. Despite explaining the extent of my involvement in the tsunami and repeated suicide attempts, no doctor prior to 2011 assessed me for PTSD.
Instead of receiving appropriate treatment, I was prescribed antidepressants. These only made me feel worse. They reminded me daily that I couldn’t cope, deepening my feelings of helplessness. When I skipped doses, I felt better simply because I wasn’t constantly reminded of the trauma.
Why cannabis became a coping mechanism
In the absence of proper treatment, I turned to smoking cannabis before sleep, which helped with the nightmares and allowed me to sleep consistently. Instead of seeing it as a coping mechanism, medical professionals and others blamed cannabis for my issues, even accusing me of using PTSD as an excuse for my behavior.
My Turning Point: Diagnosis and Proper Treatment
It wasn’t until October 2011, thanks to Dr. Richard Simpson’s intervention, that I was formally diagnosed with PTSD. After this diagnosis, my treatment drastically improved. When I was referred to the Crisis Team in January 2012, the treatment approach was completely different. The nurses were now instructed on my diagnosis and were trained to help me with day-to-day tasks without forcing me to relive the trauma. This marked a huge shift in my care and is a testament to how much early diagnosis could have changed my trajectory.
Looking Back: Lessons Learned and Thoughts on the NHS
The NHS system was not equipped to help me at my most vulnerable. The brief GP appointments, lack of PTSD-specialized care, and dismissive attitudes made me lose faith in the system. There were countless opportunities to identify my condition and provide the proper care, but they were missed.
However, the stark contrast in care after my diagnosis in 2011 highlights that change is possible. Early intervention is critical. My journey could have been far less painful if someone had recognized the signs sooner and provided the appropriate help.
Reflections for Those Still Struggling
If you are experiencing trauma, whether it’s from a natural disaster, conflict, or any other life-changing event, know this: PTSD is real. It can be silent, inconsistent, and incredibly isolating, but it’s not a reflection of weakness. I urge anyone who feels misunderstood by medical professionals to seek a second opinion or push for a proper diagnosis.
There are more resources available now than ever before for those dealing with PTSD. Whether through therapy, peer support, or advocacy groups, healing is possible—but the first step is getting the right diagnosis.
Helpful Resources:
Final Thoughts
It took years of misdiagnosis, dismissiveness, and misunderstanding before I finally got the help I needed. But I’m still here, and I’m sharing this story not just for me, but for anyone who feels lost in the system. Advocate for yourself, push for the care you deserve, and don’t give up. Healing is a long road, but you don’t have to walk it alone.




0 Comments